Medicine case cervical spondyloarthropathy
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case discussion:
A 60 year old female from annaram presented with cheif complaints of
- headache and neck pain
- giddiness
- slurred speech
Since 7days.
HOPI-
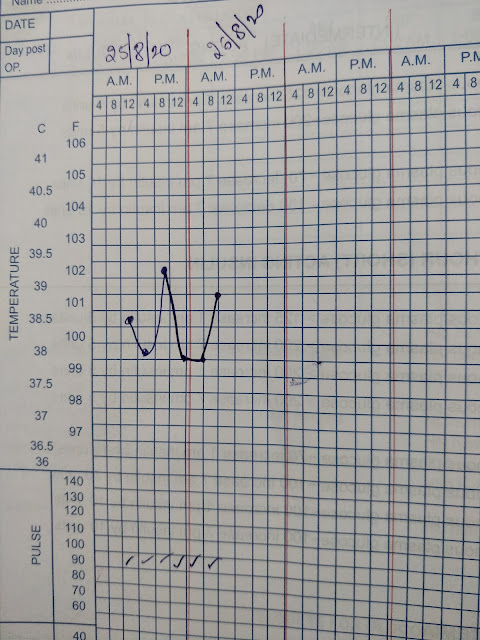
She was apparently asymptomatic till 17-7-20,then she developed fever on 18-7-20 which is high grade , intermittent ,not associated with chills and rigors.
She went to local hospital and got medication for fever which subsided in 2 days.It was associated with 1 episode of vomiting.
On 19-7-20 she developed headache,neck pain and lower backache. The speech became slurred.
On 20-7-20 as the pain was not relieved with medications given by rmp and doctors in Suryapet she was referred to kamineni.
On 21-7-20 patient came to casualty with Neck pain which was non radiating,with restricted neck movements,no aggregating and relieving factors.
No history of throat pain,ear pain,nasal discharge and difficulty in deglutition.
Headache was associated with giddiness.
There is no history of photophobia and phonophobia.
No history of difficulty in swallowing, decreased word output,loss of consciousness and seizures.
No history of blurring of vision,diplopia, deviation of mouth, drooling of saliva
No history of trauma
PAST HISTORY
Past medical- unilateral swelling of left leg till knee, initially she had developed fever later the swelling got progressed over 10-15 days fow which she took local treatment but there was no improvement.There is a history of community spread of swelling of limbs.
Not a known case of DM, Hypertension, asthma, epilepsy,CHD and CKD.
Life before hospital-
Born in sarvaram ,married at the age of 9 yrs ,came to annaram with her husband.She has 4 children- 2 sons and 2 daughters through normal vaginal delivery.
Past surgeries-family planning operation at the age of 30 yrs, hysterectomy done 24yrs back, post op -uneventful.
No history of blood transfusion.
PERSONAL HISTORY
Diet- mixed,leg used to swell whenever she eats sour foods.
Appetite- normal
Sleep- adequate
Bladder- regular
Bowel-irregular, sometimes she used to pass stools once in 5 days like hard pellets.
Addictions- toddy since her 15 yrs,chutta 10yrs.
Siblings-2 sisters and 1 brother,One of her sisters had complaints of severe headache since her childhood for which she uses self medications.
Parents-father died at the age of 20 yrs,mother died last yr cause of death-fever,did not take any medications.
Marriage at 9yrs of age
Father's death at 20 yrs of age
Family planning operation at 30 yrs of age
Hysterectomy at 36yrs
Filariasis at 50 yrs
FAMILY HISTORY
No similar complaints in the family.
DRUG HISTORY
Not allergic to any known drugs.
TREATMENT HISTORY






Comments
Post a Comment